Upgrade to High-Speed Internet for only ₱1499/month!
Enjoy up to 100 Mbps fiber broadband, perfect for browsing, streaming, and gaming.
Visit Suniway.ph to learn
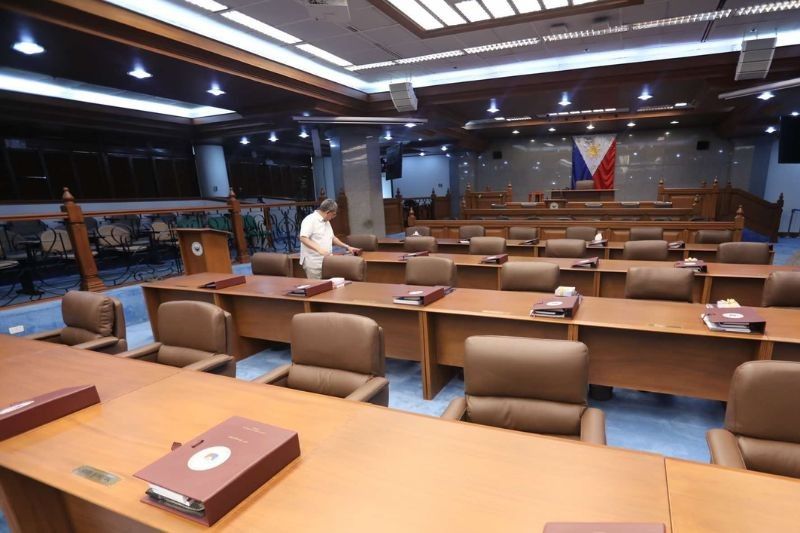
MANILA, Philippines — The Supreme Court has ruled that a physician who properly advises a patient, explains the risks of a procedure and obtains informed consent cannot be held liable for medical malpractice if complications occur.
In a 22-page decision promulgated on April 2, 2025, the high court upheld the dismissal of a complaint filed against physician Avelino Aventura, head of the Philippine Heart Center’s (PHC) Surgery Department, over the death of his patient, Quintin Que, in 2000 following a failed stenting procedure.
Que was initially referred to Aventura due to hoarseness, which was later diagnosed as an aneurysm in the aortic arch affecting his vocal cords. A CT scan confirmed the life-threatening condition.
After conducting several tests, Aventura recommended a heart bypass operation, with plans to treat the aneurysm later. The bypass surgery was successfully performed.
Months later, when the aneurysm worsened, Aventura presented two treatment options: open-chest surgery or a newer, less invasive stenting procedure.
The Que family initially hesitated but eventually consented to the stenting, which was presented as generally safer and with fewer complications.
Aventura clarified that the procedure still carried risks, including death, and that he would not perform the operation himself since it was beyond his specialization.
The Que family consented to proceed under the care of physician Eric Verhoeven, a visiting Belgian specialist.
On the day of the operation, Verhoeven attempted to insert the custom stent three times but was unsuccessful due to a bend in the artery. Following these attempts, Quintin suffered a stroke and never regained consciousness. The family was informed the stent was "faulty."
The patient died on Feb. 27, 2000. An autopsy performed by forensic pathologist physician Raquel Fortun concluded that Quintin died from complications of hypertensive atherosclerotic cardiovascular disease, triggered by catheterization, a natural cause of death.
The family later discovered that Verhoeven was not licensed to practice medicine in the Philippines. This led Quintin’s son, Elpidio Que, to file a complaint for damages against Aventura, Verhoeven and the PHC, accusing them of medical malpractice.
The case was dismissed by the Regional Trial Court for lack of merit, a ruling later affirmed by the Court of Appeals. Elpidio then elevated the case to the Supreme Court.
High court ruling. In denying the petition, the Supreme Court said there was no merit in the claim of medical negligence.
It emphasized that Aventura fulfilled his duty of care by adequately informing the family of the procedure’s risks and seeking informed consent. The court noted that while stenting posed fewer risks than open surgery, it was not risk-free.
“The facts show that Dr. Aventura informed the Que family, most especially Quintin, of the material risks inherent in the stenting procedure, including the risk of death,” the decision read.
The court also noted that Aventura had disclosed that another physician, not him, would perform the procedure, as it was outside his field of expertise.
Expert witnesses, including cardiovascular and endovascular surgeons, testified that stenting was a medically reasonable and appropriate choice for Quintin’s condition given the alternatives.
In dismissing the case, the high court reiterated that adverse medical outcomes do not automatically constitute negligence, especially when risks are communicated, consent is obtained and care is properly administered.

 4 hours ago
2
4 hours ago
2